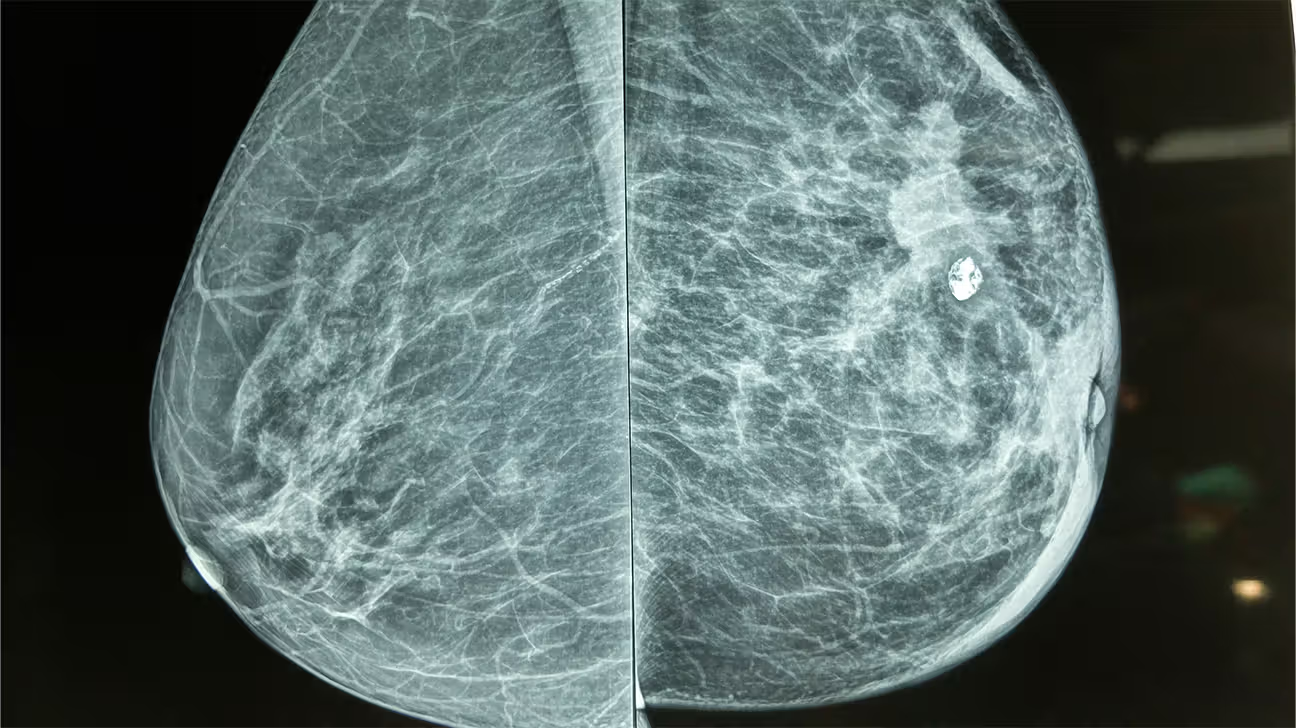
The relationship between breast implants and mammography is not one of simple obstruction, but rather a complex technical challenge that requires a specialized approach to maintain the efficacy of cancer screening. Many individuals and even some general practitioners hold the misconception that breast augmentation renders mammography ineffective or excessively risky, leading to unnecessary anxiety or, worse, a reluctance to pursue essential annual screenings. The reality is that while the presence of a foreign object—whether saline or silicone—does fundamentally alter the physics of X-ray imaging and the necessary compression techniques, modern radiology has developed specific, validated protocols to mitigate these issues. The core problem revolves around the radio-opacity of the implant material, which casts a dense white shadow on the mammographic film, potentially obscuring a critical percentage of the surrounding breast parenchyma where cancerous lesions might develop. This challenge, however, has been systematically addressed through standardized views and supplementary imaging modalities.
The core problem revolves around the radio-opacity of the implant material, which casts a dense white shadow on the mammographic film
The most significant and widely discussed factor is the physical barrier the implant creates between the X-ray source and the detector. Because both silicone and saline implants are substantially denser than natural glandular and fatty breast tissue, they absorb a greater amount of the X-ray energy, resulting in the aforementioned white shadow. This shadowing effect is not trivial; depending on the size and placement of the implant, studies have estimated that between 20% to over 80% of the natural breast tissue, particularly the posterior aspects near the chest wall, can be visually obscured on standard mammographic projections. Without specialized positioning, this reduced visibility creates an area of concern, as a small, developing tumor within the shadowed zone could be missed. This underscores the necessity of a tailored procedure rather than a generic screening protocol.
This shadowing effect is not trivial; depending on the size and placement of the implant, studies have estimated that between 20% to over 80% of the natural breast tissue… can be visually obscured
To counteract the implant’s obscuring effect, a specialized technique known as the Eklund view, or implant displacement view (ID), was introduced and has since become the globally recognized standard of care. This technique involves a skilled mammography technologist using gentle, focused pressure to push the implant posteriorly, toward the chest wall, while pulling the natural breast tissue forward and away from the implant. The separated tissue is then compressed and imaged independently, allowing for a much clearer visualization of the anterior and central breast parenchyma without the dense implant shadow overlay. This maneuver effectively doubles the number of images taken during a typical screening—from four standard views to eight (four standard views plus four ID views)—and is crucial for maximizing the amount of visible glandular tissue for radiological assessment. Crucially, the proper execution of the Eklund technique compresses only the breast tissue, not the implant itself, making the risk of implant rupture during the procedure exceedingly low, especially with modern, cohesive gel devices.
This technique involves a skilled mammography technologist using gentle, focused pressure to push the implant posteriorly, toward the chest wall, while pulling the natural breast tissue forward and away from the implant.
The positioning of the implant relative to the chest muscle also profoundly influences the ease and efficacy of the Eklund technique. Implants placed subglandularly (above the pectoral muscle) tend to be more mobile and can often be displaced more easily for the ID views, which in theory allows the technologist to capture a greater volume of the posterior breast tissue. Conversely, subpectoral placement (partially or fully beneath the chest muscle) can render the implant more securely fixed, sometimes making the necessary displacement more challenging to execute successfully. While subpectoral placement was once thought to universally offer a better view of the breast tissue, the technical execution and outcome are often dependent on the patient’s individual anatomy and the degree of capsular contracture, or hardening of the tissue around the implant, which can limit the implant’s mobility regardless of its initial position.
The positioning of the implant relative to the chest muscle also profoundly influences the ease and efficacy of the Eklund technique.
Beyond the visibility issue, there is the concurrent need to assess the integrity of the implant itself during the screening process. While mammography is the gold standard for breast tissue evaluation, it is not the most sensitive tool for detecting subtle or contained implant ruptures, particularly in the case of silicone implants. Saline implants, when ruptured, are typically obvious due to the rapid deflation of the shell, but a slow, intracapsular rupture of a silicone implant (where the silicone remains contained by the fibrous capsule) can be “silent” and missed on mammography because the dense silicone gel simply continues to cast a uniform shadow. For this specific concern, supplementary imaging, such as a dedicated breast ultrasound or, more definitively, a magnetic resonance imaging (MRI) scan, is often recommended, especially for women with silicone implants or those experiencing symptoms like changes in breast contour or hardness.
While mammography is the gold standard for breast tissue evaluation, it is not the most sensitive tool for detecting subtle or contained implant ruptures.
The advent of Digital Breast Tomosynthesis (DBT), often referred to as 3D mammography, introduces a new layer of complexity and potential benefit for augmented breasts. DBT captures a series of low-dose X-ray images from various angles, which are then reconstructed by a computer to create a pseudo-3D volume of the breast tissue. This technology is excellent for reducing the effect of overlapping tissues, which is a common issue even in non-augmented, dense breasts. While it may offer a clearer view of the tissue that is successfully displaced in an Eklund view, it does not fully solve the core problem of the implant’s shadow, as the implant still obscures the most posterior tissue. Nevertheless, the improved clarity in the visualized tissue, coupled with standard Eklund views, can improve diagnostic accuracy and potentially reduce the rate of recall for additional imaging compared to traditional 2D mammography.
The advent of Digital Breast Tomosynthesis (DBT), often referred to as 3D mammography, introduces a new layer of complexity and potential benefit for augmented breasts.
A historical concern that has largely been debunked by extensive epidemiological research is the notion that the implants themselves increase the inherent risk of developing breast cancer. Major meta-analyses and long-term cohort studies have consistently demonstrated that women with cosmetic breast implants—whether saline or silicone—do not have a higher incidence rate of the most common types of breast carcinoma compared to the general population. The critical factor for these women is not an altered biological risk, but the potential for a delayed diagnosis due to the challenge of proper imaging. This makes adherence to the established screening guidelines, and being insistent about receiving the specialized Eklund views at a facility experienced in imaging augmented breasts, absolutely non-negotiable for long-term health surveillance.
A historical concern that has largely been debunked by extensive epidemiological research is the notion that the implants themselves increase the inherent risk of developing breast cancer.
Ultimately, the onus is on the patient to communicate clearly with their healthcare provider and the imaging facility. Women with breast implants must actively inform the scheduling staff and the technologist of their augmentation status, the type of implant, and its placement (subglandular or subpectoral). This ensures that the appropriate amount of time is allotted for the specialized Eklund views and that the examination is performed by personnel who possess the requisite skill and experience. Failure to provide this information can result in a suboptimal standard mammogram that offers a false sense of security due to the substantial amount of obscured tissue. Screening for cancer remains a priority, and with the proper technique, the challenge presented by breast implants is a manageable one.
Women with breast implants must actively inform the scheduling staff and the technologist of their augmentation status, the type of implant, and its placement.
The presence of breast implants necessitates a modified mammography protocol, specifically the Eklund view, to counter shadowing and ensure comprehensive, effective breast cancer screening.
